Cognitive behavioral therapy (CBT) is a form of effective psychological treatment for depression, anxiety disorders, alcohol and drug use problems, marital problems, eating disorders, and severe mental illness.
Numerous research studies suggest that CBT leads to significant improvement in functioning and quality of life. In many studies, CBT has been demonstrated to be as effective as, or more effective than, other forms of psychological therapy or psychiatric medications, referenced at ada.org.
According to the American Psychological Association, the core concepts of CBT include:
- psychological issues are partly based on unhelpful ways of thinking
- psychological issues are partly based on learned patterns of behavior
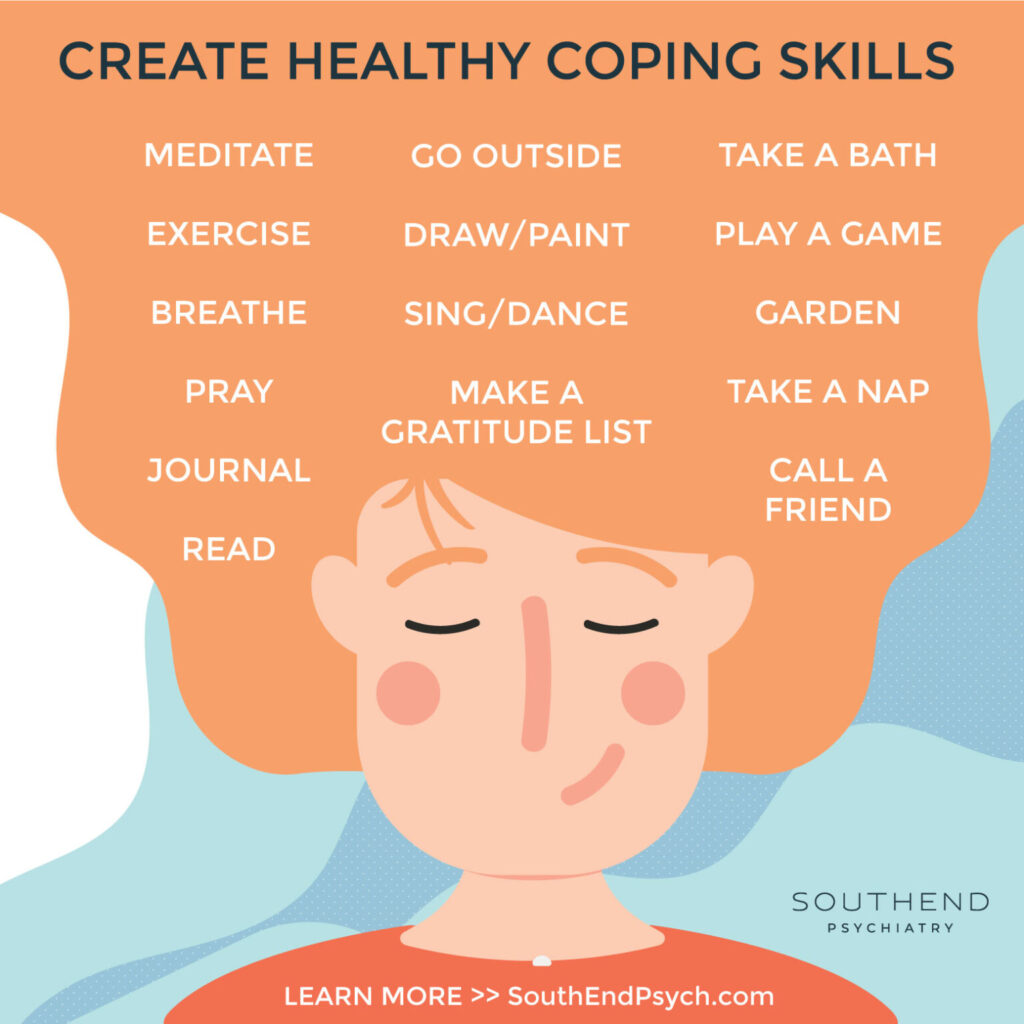
- those living with these issues can improve with better coping mechanisms and management to help relieve their symptoms
Healthline provides some of the most popular techniques used in CBT:
- SMART goals. SMART goals are specific, measurable, achievable, realistic, and time-limited.
- Guided discovery and questioning. By questioning the assumptions you have about yourself or your current situation, your therapist can help you learn to challenge these thoughts and consider different viewpoints.
- Journaling. You might be asked to jot down negative beliefs that come up during the week and the positive ones you can replace them with.
- Self-talk. Your therapist may ask what you tell yourself about a certain situation or experience and challenge you to replace negative or critical self-talk with compassionate, constructive self-talk.
- Cognitive restructuring. This involves looking at any cognitive distortions affecting your thoughts — such as black-and-white thinking, jumping to conclusions, or catastrophizing — and beginning to unravel them.
- Thought recording. In this technique, you’ll record thoughts and feelings experienced during a specific situation, then come up with unbiased evidence supporting your negative belief and evidence against it. You’ll use this evidence to develop a more realistic thought.
- Positive activities. Scheduling a rewarding activity each day can help increase overall positivity and improve your mood. Some examples might be buying yourself fresh flowers or fruit, watching your favorite movie, or taking a picnic lunch to the park.
- Situation exposure. This involves listing situations or things that cause distress, in order of the level of distress they cause, and slowly exposing yourself to these things until they lead to fewer negative feelings. Systematic desensitization is a similar technique where you’ll learn relaxation techniques to help you cope with your feelings in a difficult situation.
How CBT Can Help
Healthline states that typical CBT treatment often involves the following:
- recognizing how inaccurate thinking can worsen problems
- learning new problem-solving skills
- gaining confidence and a better understanding and appreciation of your self-worth
- learning how to face fears and challenges
- using role play and calming techniques when faced with potentially challenging situations
The goal of these techniques is to replace unhelpful or self-defeating thoughts with more encouraging and realistic ones.
CBT can help with a range of things, including:
- depression
- substance misuse
- post-traumatic stress disorder (PTSD)
- anxiety disorders, including panic disorder and phobia
- obsessive-compulsive disorder (OCD)
- schizophrenia
- bipolar disorder
- eating disorders
CBT can also help with:
- grief and loss
- chronic pain
- insomnia
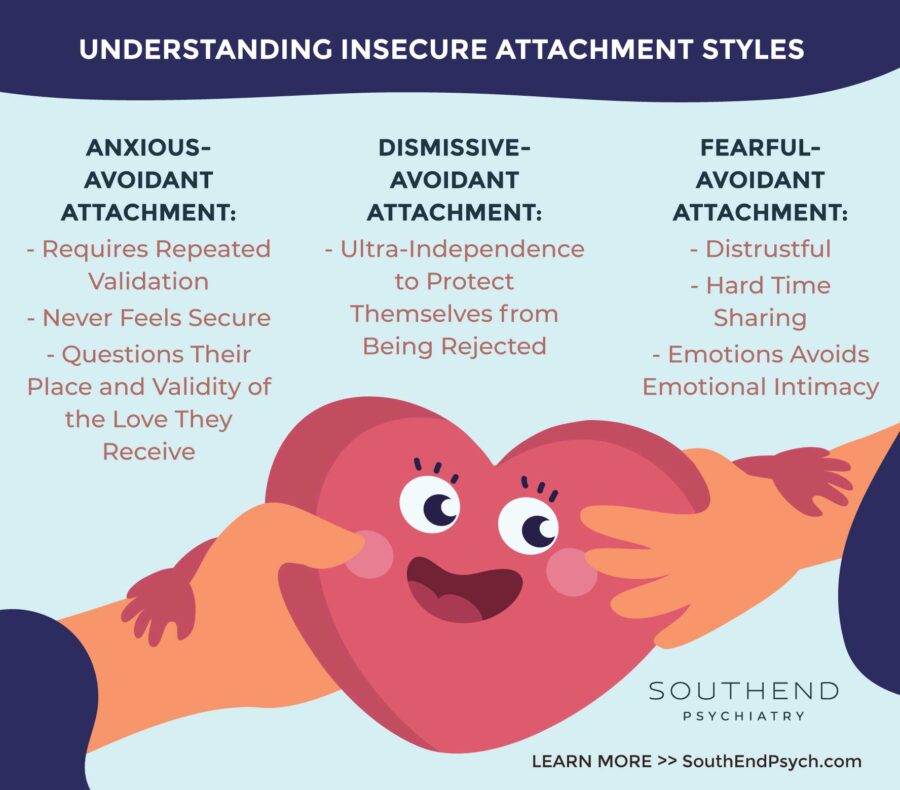
- relationship difficulties like a breakup or divorce
- a serious health diagnosis, such as cancer
If you are interested in Cognitive Behavioral Therapy, SouthEnd Psychiatry is here for you. Our amazing team of licensed therapists are ready to walk along side you in this journey.
Contact Southend Psych today to inquire about appointment availability and get you on your way to a better place.
Southend Psychiatry
Schedule your appointment today with one of our SouthEnd Psychiatry clinicians. Book your appointment online or call 1-800-632-7969 to get started today.