Suicide is a complex and deeply troubling issue that affects millions of people around the world. It is a leading cause of death, particularly among young adults, and leaves behind a ripple effect of pain and loss for families, friends, and communities. We at SouthEnd Psychiatry understand that while the causes of suicide are multifaceted, involving a combination of mental health struggles, life stressors, and sometimes a sense of hopelessness, one critical factor in prevention is the role of community support.
Understanding Suicide: A Global Challenge
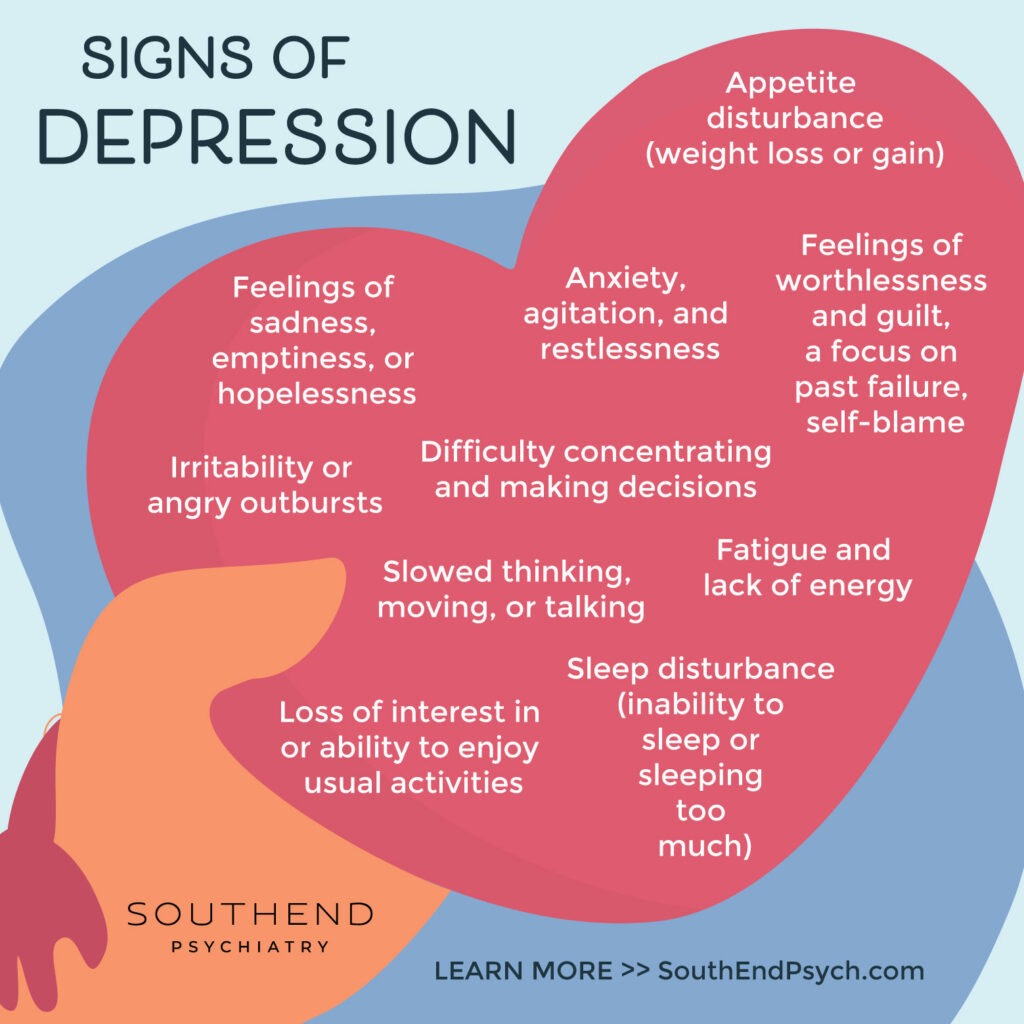
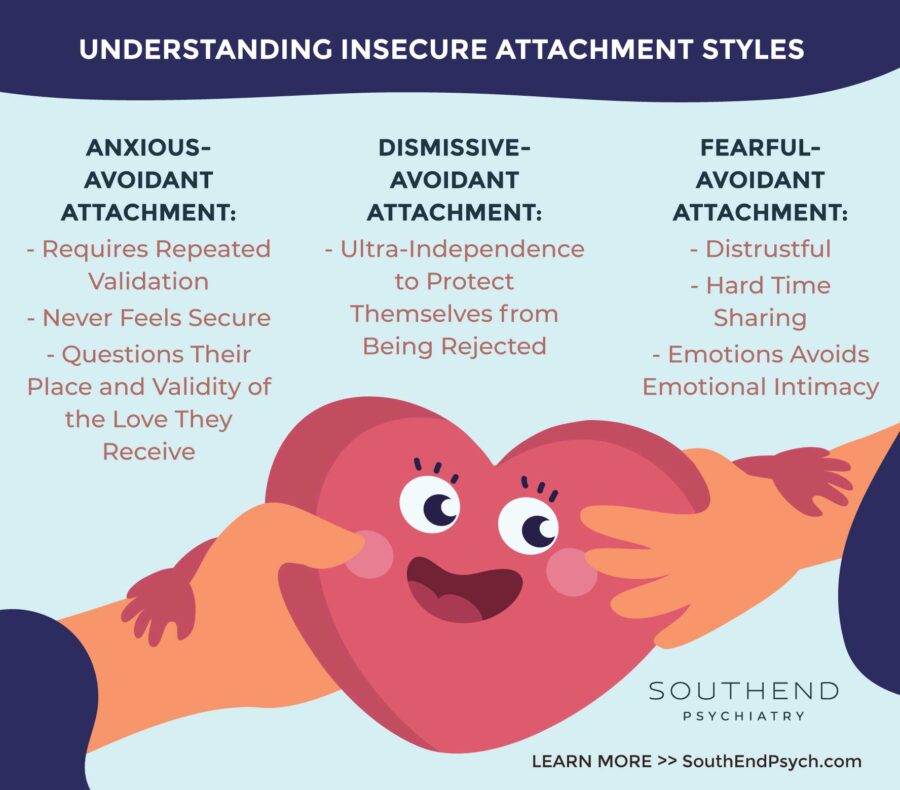
Suicide is often the result of a convergence of factors, including mental illness (such as depression, anxiety, and bipolar disorder), substance abuse, trauma, and severe life stressors like financial problems, relationship issues, or chronic illness. In many cases, individuals who are contemplating suicide feel isolated, believing that they are alone in their pain or that their situation is hopeless.
Despite its prevalence, suicide remains a taboo subject, often shrouded in stigma and misunderstanding. This stigma can prevent people from seeking help, further isolating those who are already struggling. It is essential to break this silence and foster open, compassionate conversations about mental health and suicide prevention.
The Power of Community: A Lifeline for Those in Need
Community support plays a crucial role in suicide prevention. Strong, supportive communities can provide individuals with the connections, resources, and encouragement they need to navigate difficult times. Here’s how community can make a difference:
- Creating a Sense of Belonging: Feeling connected to others is a fundamental human need. Communities that foster inclusivity, empathy, and understanding can help individuals feel valued and supported, reducing feelings of isolation and loneliness.
- Providing Emotional Support: Having someone to talk to can be life-saving. Friends, family, and community members who offer a listening ear without judgment can help those struggling with suicidal thoughts feel understood and less alone.
- Raising Awareness and Reducing Stigma: Communities that actively promote mental health awareness and openly discuss suicide can help reduce the stigma associated with seeking help. Education and outreach programs can empower individuals to recognize the signs of suicidal behavior in others and encourage them to intervene.
- Connecting People to Resources: Communities are often gateways to essential resources, such as mental health services, crisis hotlines, and support groups. By knowing where to turn for help, individuals in crisis are more likely to access the support they need.
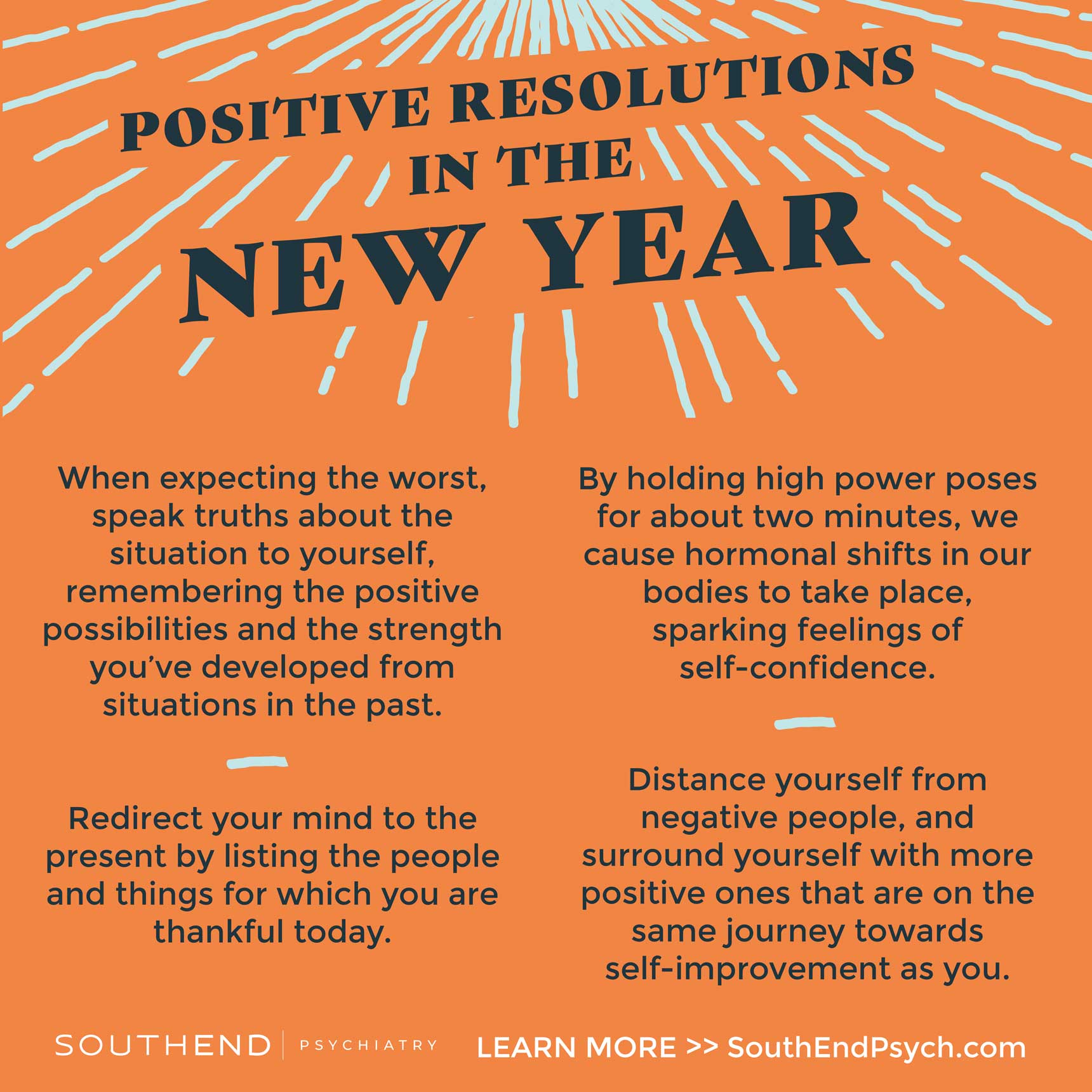
- Encouraging Healthy Coping Mechanisms: Communities can promote activities and environments that encourage healthy coping mechanisms, such as physical exercise, creative outlets, and mindfulness practices. These activities can help individuals manage stress and emotional pain more effectively.
- Building Resilience: Through shared experiences and collective support, communities can help individuals build resilience, teaching them how to navigate life’s challenges and bounce back from adversity.
How to Foster a Supportive Community
- Start the Conversation: Encourage open dialogue about mental health and suicide prevention. By talking openly, you can help break down the stigma and make it easier for others to seek help.
- Offer Support and Listen: Be present for those around you. Sometimes, simply listening and showing empathy can make a huge difference to someone in need.
- Educate Yourself and Others: Learn about the signs of suicide and how to respond if someone you know is struggling. Share this knowledge with your community to empower others to help as well.
- Promote Mental Health Resources: Share information about local mental health services, hotlines, and support groups. Make it easy for people to find help when they need it.
- Create Safe Spaces: Whether it’s a physical location or a virtual group, creating spaces where people feel safe to express their feelings and seek support can be incredibly valuable.
The Lifesaving Impact of Community
Suicide is a preventable tragedy, but it requires the collective effort of communities to create a supportive environment where individuals feel safe to seek help. By fostering connections, reducing stigma, and promoting awareness, communities can play a vital role in saving lives and supporting those in need. Together, we can make a difference and provide hope to those who may be struggling in silence.
Are you struggling right now? Our team at SouthEnd is here and ready to help. We invite you to start a conversation with us, on your terms, in-person or online and want you to know you’re not alone.
Southend Psychiatry
Schedule your appointment today with one of our SouthEnd Psychiatry clinicians. Book your appointment online or call 1-800-632-7969 to get started today.