May is Mental Health Awareness Month and we are excited to join the National Alliance on Mental Illness (NAMI) in promoting this year’s theme, “More Than Enough” which is meant to be a message of hope and inclusion.
No matter where you are in your mental health journey, you are deserving of support, resources, fulfillment and a community that cares about you… no matter what you look like or what you are able and not able to do.
Build Connection and Community
People living with mental health conditions need to know and feel valued and supported by their communities. It is important to start conversations and share resources to raise awareness of how critical this topic is.
“While some are lucky to have a community that understands the reality of mental illness, that doesn’t mean that everyone we encounter has risen above the pervasive stigma. Sometimes, making progress requires having tough conversations.” Margot Harris, Associate Editor of Marketing at NAMI
Education and Advocacy
This month, help us educate people on mental health issues and challenges as well as help empower new and current advocates to help advocate for the rights people affected by mental health conditions deserve. Here are a few statistics to help bring this concept to reality:
- 1 in 5 U.S. adults experience a mental health condition each year.
Annually, mental illness affects:
- 16% of Asian adults
- 21% of Black/African American adults
- 18% of Native Hawaiian/Pacific Islander adults
- 21% of Hispanic adults
- 27% of American Indian/Alaska Native adults
- 24% of White adults
- 35% of multiracial adults
- 50% of LGB adults
Creating Awareness and Driving Action
We can increase awareness of mental health support and advocacy by taking real action this month! By continuing to learn more about this topic and getting involved in local events and initiatives, we can make a difference.
- ACT: send an email, share a story, or post on social media to urge your elected officials to support mental health. Visit https://nami.quorum.us/AdvocacyAlerts for details.
- VOTE: commit to understanding how your vote impacts people with mental health conditions. Visit: https://www.vote4mentalhealth.org to get started.
- JOIN: Many virtual and in-person NAMIWalks will be taking place throughout the country during the month of May to help bring awareness and spread the message of Mental Health for All! Promote NAMIWalks events taking place in your local areas. Encourage people to use their creativity, create teams and participate however they can. Visit https://www.namiwalks.org/ to find events in your area.
Together, we can make a difference and realize our shared vision of a nation where anyone affected by mental illness can get the appropriate support and quality of care to live healthy, fulfilling lives. Help us spread the word through awareness, support and advocacy activities.
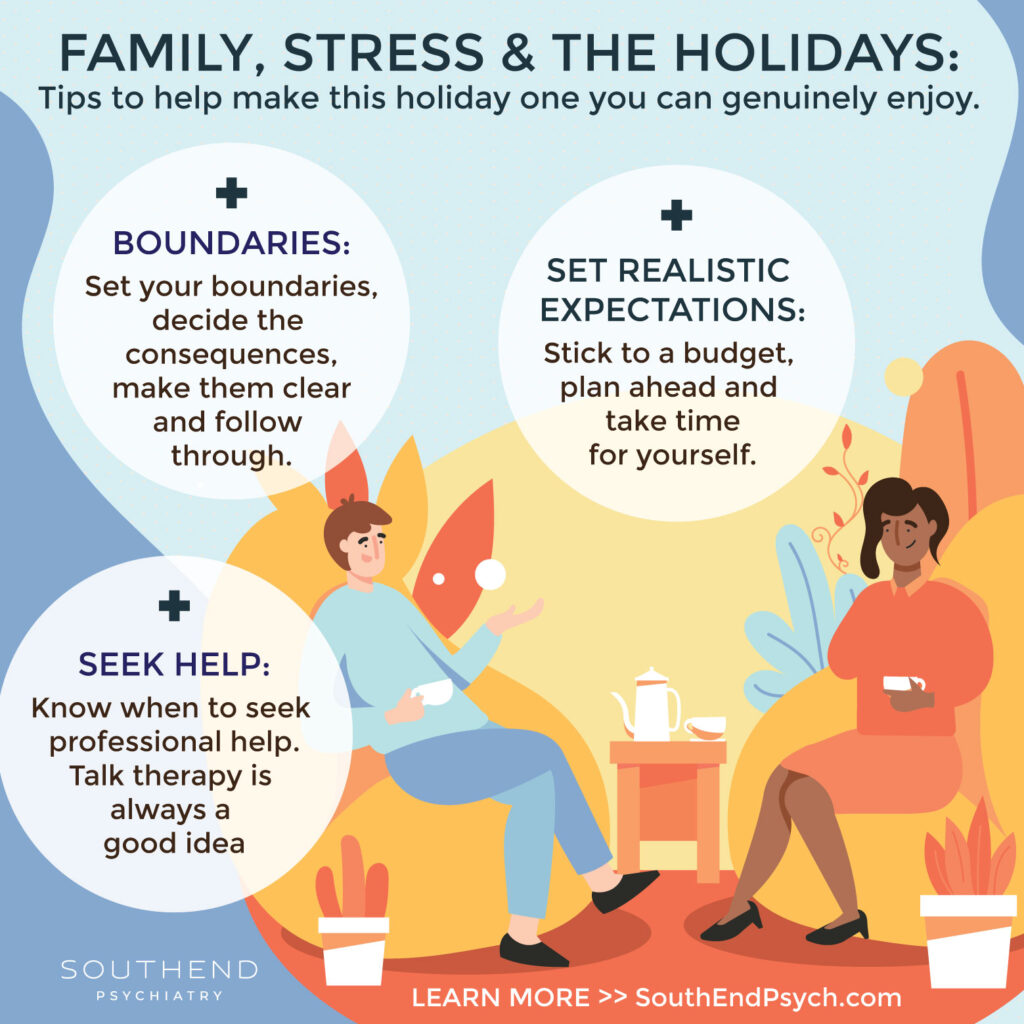
Southend Psychiatry is here as you navigate this journey. We can come alongside you to offer support and help. Contact Southend Psych today to inquire about appointment availability and get on your way to a better you.
Southend Psychiatry
Schedule your appointment today with one of our SouthEnd Psychiatry clinicians. Book your appointment online or call 1-800-632-7969 to get started today.