As the days grow shorter and the temperatures drop, many people find themselves feeling a bit more tired, unmotivated, or down than usual. For some, however, these seasonal changes bring on a deeper and more profound sense of sadness, lethargy, and withdrawal—a condition known as Seasonal Affective Disorder (SAD). SAD is a type of depression that follows a seasonal pattern, most often occurring in the fall and winter months. Understanding the symptoms of SAD and exploring effective ways to manage it can make a significant difference for those affected by this condition.
At Southend Psychiatry, we’re here to help you recognize the signs of SAD and provide support through therapies, lifestyle changes, and treatment options that can bring relief and restore balance during the darker months.
Recognizing the Symptoms of Seasonal Affective Disorder
Seasonal Affective Disorder often begins in late fall and can persist until spring. Its symptoms can range from mild to severe and typically include:
- Low Mood: Persistent feelings of sadness, hopelessness, or apathy.
- Lethargy and Fatigue: A strong sense of tiredness and low energy, even after a full night’s sleep.
- Increased Sleep: A tendency to sleep more than usual, often feeling like it’s never enough.
- Weight Gain and Appetite Changes: Increased cravings for carbohydrates and comfort foods, which can lead to weight gain.
- Social Withdrawal: Reduced interest in social activities, hobbies, and connections with others.
- Difficulty Concentrating: A feeling of “brain fog” or trouble focusing on tasks.
These symptoms can disrupt daily life, making it difficult to maintain routines, work effectively, and engage in relationships. While it’s normal to feel some adjustment as the seasons change, people with SAD experience symptoms that significantly impact their quality of life.
What Causes Seasonal Affective Disorder?
Although the exact causes of SAD are still being studied, several factors appear to contribute to this condition:
- Reduced Sunlight Exposure: Shorter days and less sunlight can disrupt your body’s internal clock, leading to feelings of fatigue and depression. Sunlight exposure plays a crucial role in regulating mood by impacting serotonin production and melatonin levels.
- Circadian Rhythm Disruption: Our bodies rely on sunlight to maintain a consistent sleep-wake cycle. When daylight hours decrease, the disruption of this natural rhythm can affect our mood and energy.
- Serotonin and Melatonin Imbalance: Reduced sunlight can lead to lower serotonin levels, impacting mood and emotional stability. Melatonin production, which helps regulate sleep, may also increase during darker months, contributing to sleepiness and lethargy.
Managing Seasonal Affective Disorder: Therapies, Lifestyle Changes, and Support Options
If you recognize the symptoms of SAD in yourself or a loved one, there are several effective treatment and management strategies to consider. Here are some approaches to help reduce the impact of SAD and enhance your mental well-being:
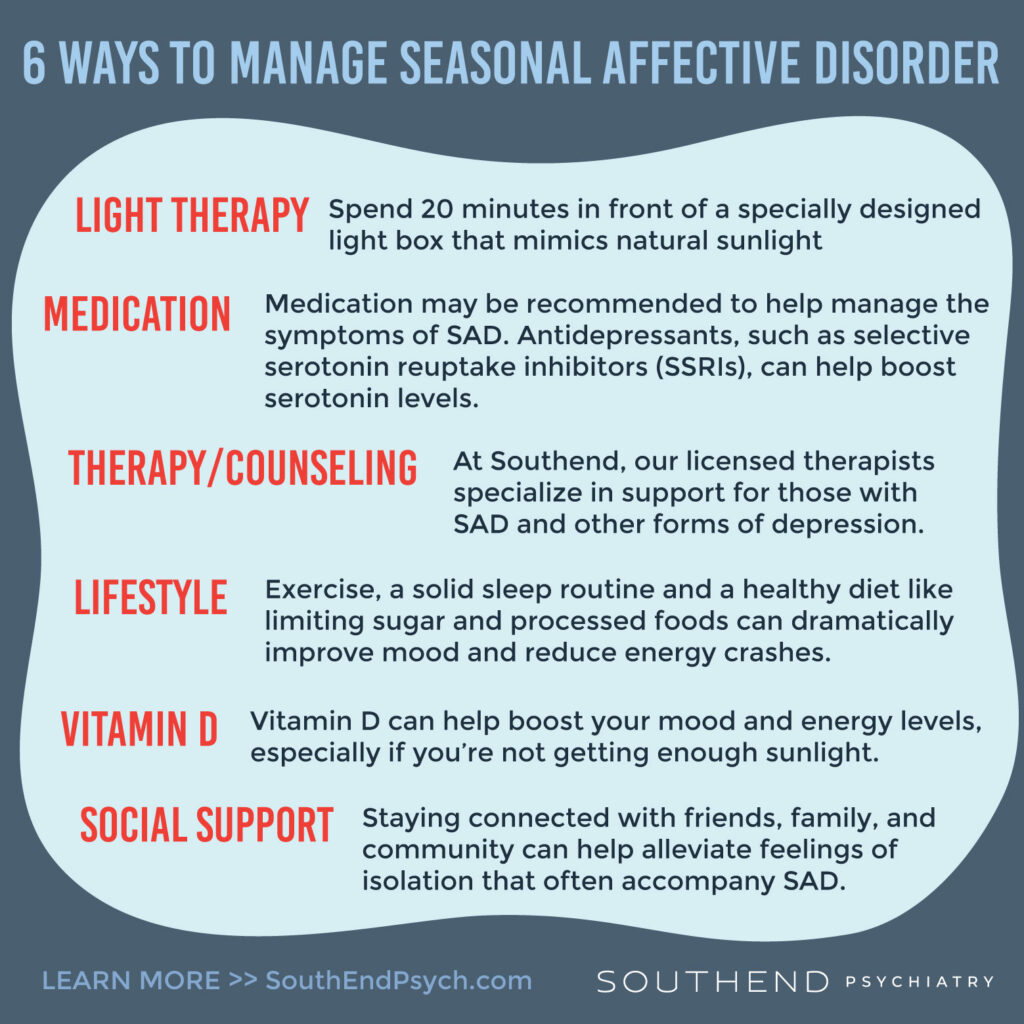
1. Light Therapy
- Light therapy is one of the most effective treatments for SAD. This involves sitting in front of a specially designed light box that mimics natural sunlight, typically for about 20-30 minutes each morning. Light therapy can help regulate your body’s sleep-wake cycle, boost serotonin levels, and alleviate symptoms of SAD.
- When using a light box, make sure to choose one with at least 10,000 lux of light and follow your doctor’s recommendations for usage.
2. Therapy and Counseling
- Cognitive Behavioral Therapy (CBT) is highly effective for treating SAD. CBT helps you identify and change negative thought patterns and behaviors that contribute to feelings of depression. Through CBT, you can develop coping skills to manage symptoms and improve your overall mental health.
- At Southend Psychiatry, our licensed therapists specialize in providing support for individuals with SAD and other forms of depression. A personalized approach to therapy can empower you to manage your symptoms more effectively.
3. Medication
- In some cases, medication may be recommended to help manage the symptoms of SAD. Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), can help boost serotonin levels and improve mood.
- If you’re considering medication, speak with a psychiatrist or healthcare provider who can assess your specific needs and help you find the most suitable treatment options.
4. Vitamin D Supplementation
- Reduced sunlight exposure during the winter months can lead to lower levels of vitamin D, which may contribute to feelings of depression. Taking a vitamin D supplement can help boost your mood and energy levels, especially if you’re not getting enough sunlight.
- Consult your healthcare provider for guidance on the right dosage for you.
5. Lifestyle Changes
- Exercise: Regular physical activity, particularly outdoors, can significantly improve mood and energy levels. Even a short walk outside on a bright winter day can make a difference.
- Healthy Diet: Focus on nutrient-dense foods, such as fruits, vegetables, lean proteins, and whole grains. Limiting sugar and processed foods can help prevent energy crashes and maintain stable blood sugar levels.
- Sleep Routine: Aim for a consistent sleep schedule by going to bed and waking up at the same time each day. Good sleep hygiene practices, such as limiting screen time before bed, can also improve your sleep quality.
6. Social Support and Connection
- Staying connected with friends, family, and community can help alleviate feelings of isolation that often accompany SAD. Even if you don’t feel like socializing, spending time with supportive people can provide comfort and lift your mood.
Don’t Let SAD Keep You in the Dark—Seek Support
If you’re struggling with symptoms of Seasonal Affective Disorder, remember that you’re not alone. SAD is a common condition, and there are effective treatments and support options available. By recognizing the signs, seeking appropriate treatment, and making small lifestyle adjustments, you can minimize the impact of SAD and enjoy a brighter, more balanced winter season.
At Southend Psychiatry, we’re committed to helping you find relief from SAD and other mental health challenges. Reach out to us today to learn more about how we can support you on your journey to better mental health.
Ready to Take Control of Your Mental Health?
If you or someone you know is struggling with Seasonal Affective Disorder, contact Southend Psychiatry for a consultation. Our experienced team of mental health professionals is here to provide personalized support and guidance. Don’t let SAD keep you from living fully—let us help you find light in the darker months.
Southend Psychiatry
Schedule your appointment today with one of our SouthEnd Psychiatry clinicians. Book your appointment online or call 1-800-632-7969 to get started today.