Summer is often seen as a season of rest and relaxation—but for many, it can bring a different kind of stress. Between coordinating family activities, juggling work responsibilities, managing kids’ summer schedules, planning vacations, and maintaining everyday life, the “mental load” can quickly become overwhelming.
What Is the Mental Load?
The mental load refers to the invisible, ongoing task of planning, remembering, and managing all the details of life—often carried by one person in a household. It’s the mental energy spent keeping track of who needs what, when things are due, and how to keep everything running smoothly.
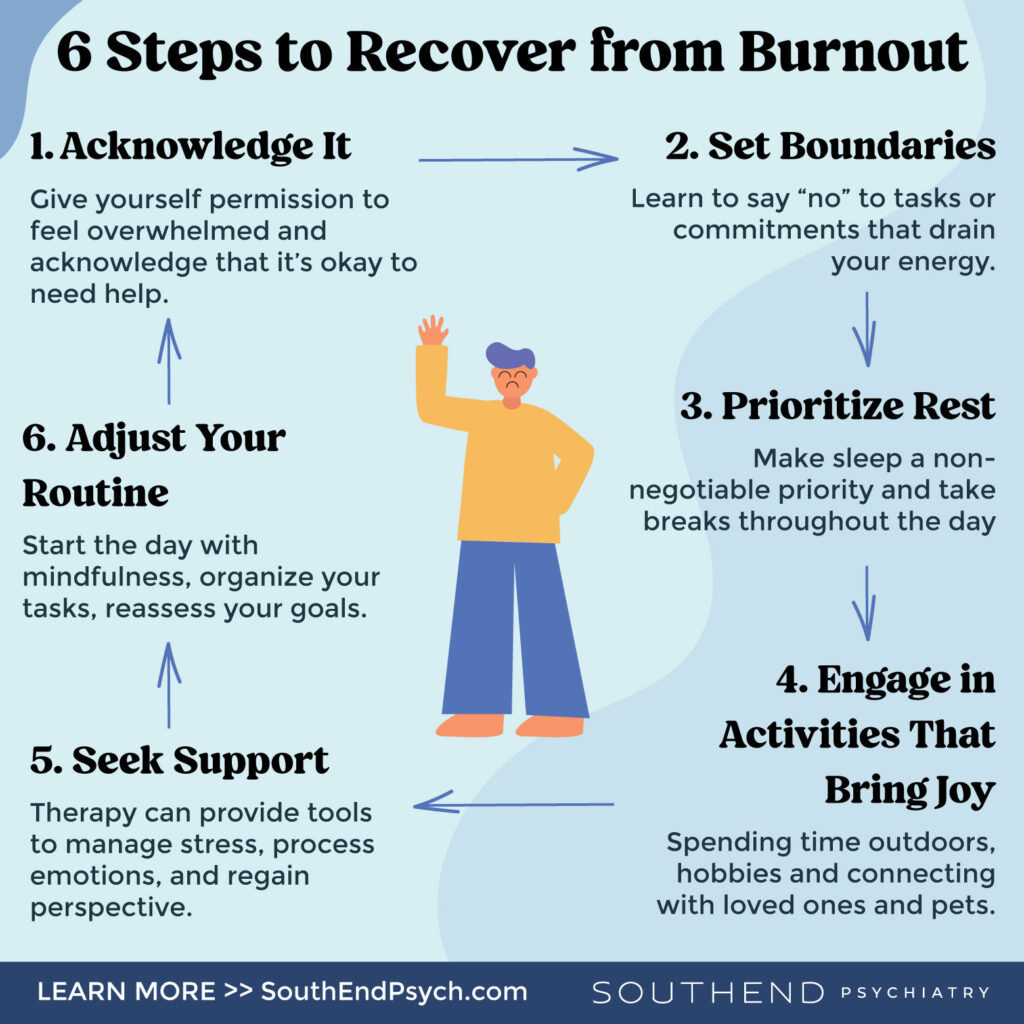
This emotional labor is often unrecognized, but it takes a toll. It can lead to anxiety, irritability, sleep issues, and even burnout—especially during high-expectation seasons like summer.
Why Summer Can Increase the Mental Load
While summer offers longer days and (hopefully) some downtime, it also presents unique challenges:
- Disrupted routines due to school being out
- Increased responsibilities like childcare or coordinating camps
- Pressure to “make the most” of the season with memorable family moments
- Balancing work and play without enough rest or recharge
How to Protect Your Peace
The good news? With awareness and intention, you can reduce the mental load and enjoy a calmer, more fulfilling summer. Here’s how:
1. Share the Load
Don’t carry it all alone. Talk openly with your partner, family, or support network about responsibilities. Delegate tasks, even the mental ones like tracking schedules or grocery lists.
2. Simplify Where You Can
You don’t need a perfect Pinterest summer. Focus on what matters most to you and your family. Say no to extra commitments that drain your energy without adding joy.
3. Schedule Recharge Time
Put quiet time on the calendar for yourself—just like appointments or events. Whether it’s a walk, a podcast, or 10 minutes with a book, prioritize activities that refill your emotional cup.
4. Set Realistic Expectations
Release the pressure to create a “perfect” summer. It’s okay for some days to be ordinary. Peace often lives in the simple, unplanned moments.
5. Talk to Someone
If your mental load is affecting your health or relationships, you don’t have to navigate it alone. Therapy can help you understand your stress, set boundaries, and develop sustainable coping strategies.
We’re Here to Support You
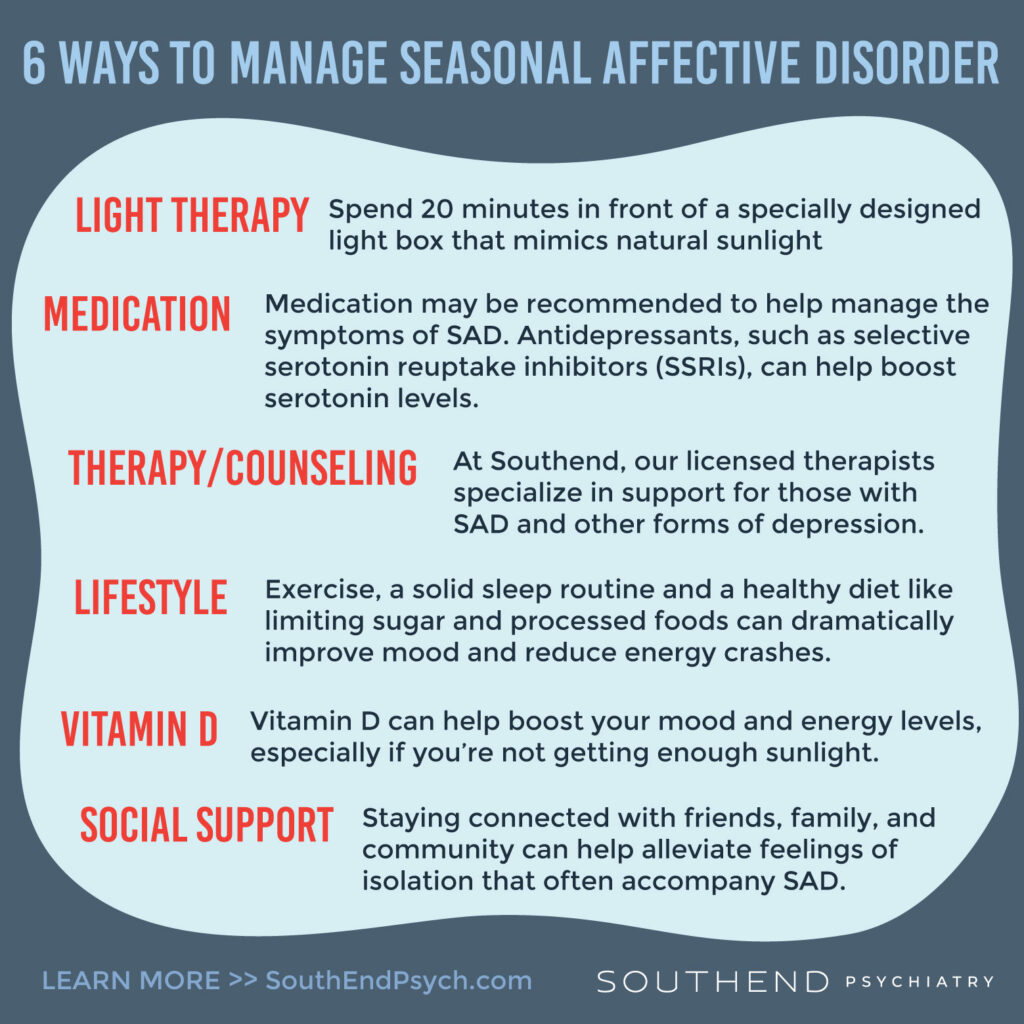
At SouthEnd Psychiatry, we understand the weight of the mental load—and we’re here to help lighten it. Whether you’re overwhelmed, burned out, or just need someone to talk to, our compassionate providers are ready to support your mental and emotional well-being this summer and beyond.
Take a step toward peace. Schedule a session today.