Every April, we observe Stress Awareness Month as a reminder to pause, reflect, and check in with ourselves. In today’s fast-paced world, stress has become a common part of daily life, affecting our health, relationships, and productivity. At Southend Psychiatry, we believe that understanding and managing stress is not just helpful—it’s essential to maintaining mental and emotional well-being.
Why Stress Awareness Matters
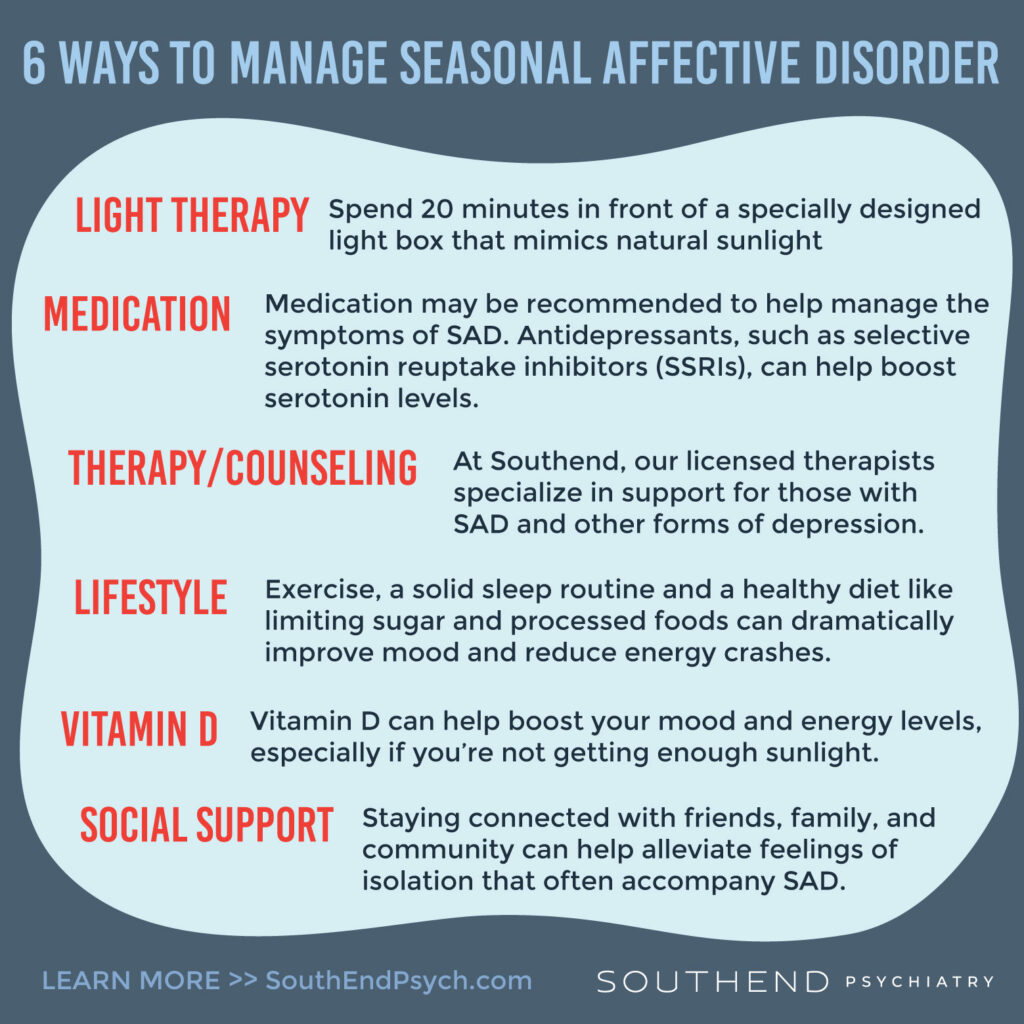
Stress, in small doses, can help us stay focused and motivated. But when it becomes chronic, it can take a serious toll on our minds and bodies. Persistent stress can lead to anxiety, depression, insomnia, high blood pressure, digestive issues, and more. That’s why it’s crucial to recognize the signs early and learn effective ways to cope.
How Southend Psychiatry Can Help
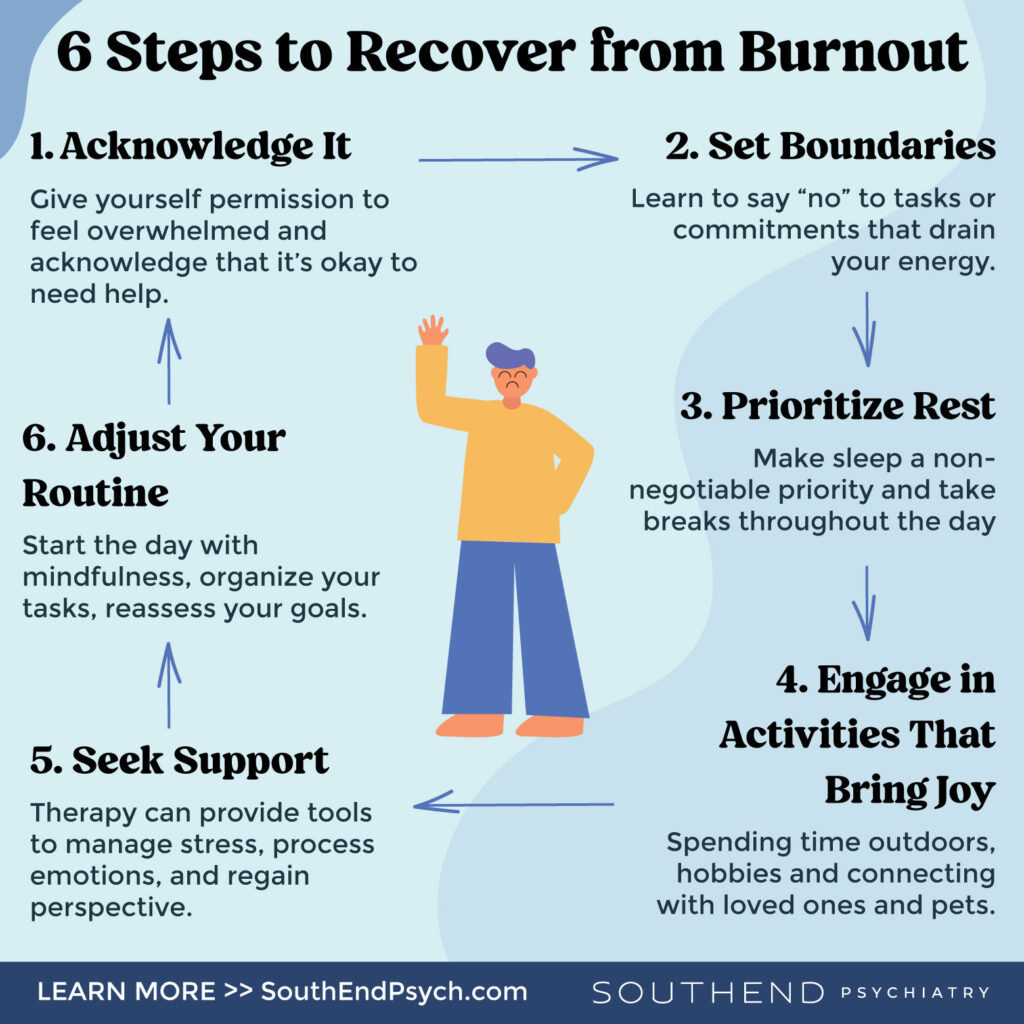
Throughout April, Southend Psychiatry is proud to offer resources, support, and practical tools to help individuals better understand and manage stress. Whether you’re dealing with workplace burnout, family pressures, or general anxiety, our team is here to help you navigate it.
Simple Techniques to Reduce Stress
Even small changes in your daily routine can have a big impact on how you feel. Here are a few quick techniques to get started:
- Deep Breathing: Take a few moments each day to breathe slowly and deeply, signaling your body to relax.
- Move Your Body: Exercise, even a short walk, can release endorphins and improve mood.
- Stay Connected: Talk with a friend, family member, or therapist—you don’t have to carry stress alone.
- Limit Screen Time: Reduce exposure to social media and news when you’re feeling overwhelmed.
- Prioritize Rest: Make time for quality sleep and restful moments throughout your day.
You Don’t Have to Manage Stress Alone
Stress is a natural part of life, but it doesn’t have to control your life. This Stress Awareness Month, we encourage you to take small steps toward a healthier, more balanced you.
If you’re feeling overwhelmed or just need someone to talk to, Southend Psychiatry is here to help. Contact us today to learn more about our services or to schedule a session with one of our compassionate providers.
Together, we can create space for healing, growth, and peace of mind.
Southend Psychiatry
Schedule your appointment today with one of our SouthEnd Psychiatry clinicians. Book your appointment online or call 1-800-632-7969 to get started today.